Reasons Why A Simpler Blood Pressure User Manual Is Imperative
- Reasons Why A Simpler Blood Pressure User Manual Is Imperative In Hindi
- Reasons Why A Simpler Blood Pressure User Manual Is Imperative Theory
- Reasons Why A Simpler Blood Pressure User Manual Is Imperative In Spanish
- Reasons Why A Simpler Blood Pressure User Manual Is Imperative 2
However normal blood pressure is having a range 120/80 in healthy people. Low blood pressure also have some symptoms and therefore it is quite easy to get an idea when you blood pressure is falling below normal. You can then check with blood pressure meter usually called Sphygmomanometer to see what the actual readings are to get a better idea. Factors that affect blood pressure (BP) variability, ie, standard deviation (SD) and variation coefficient (VC: SD/average ambulatory BP) of ambulatory BP, were examined in a community-based sample in northeastern Japan.
Abstract
Background
Patient related factors hindering optimal blood pressure (BP) control in patients with hypertension are unclear.
Objectives
To investigate the barriers to optimal hypertension management.
Methods
A survey on the awareness and management of hypertension was conducted in 556 patients (365 males, mean age 60.9 ± 10.1) from a rural community.
Results
Of the 556 patients who had a clinical diagnosis of hypertension, 127 (22.8%) were unaware the existence of the condition and received no therapy. In the 429 patients who were aware the presence of hypertension, 206 (48.0%) did not receive any antihypertensive medication at the time of this study. Fifty-four (12.5%) had a BP of less than 140/90 mm Hg. Only 21 (4.9%) received formal counselling or education from health professionals and 74 (17.2%) were aware of the optimal level of BP. Difficulty in accessing a specialist doctor was reported by 126 (29.4%). In 279 (65.0%), missing regular antihypertensive medications was reported in the 4-week period prior to this study. Omitting prescribed antihypertensive drugs due to the costs was reported by 169 (39.4%).
Conclusion
Inadequate counselling, lack of understanding on the disease, difficulties in accessing specialist care and poor medication adherence are the barriers to optimal BP control.
Introduction
Hypertension is one of the most important cardiovascular risk factors that are associated with significant complications such as coronary artery disease, stroke or renal failure. Although almost one in third of the adults may have hypertension, the awareness of this condition by the patients is low, and the control of blood pressure is generally suboptimal in rural and urban communities.–
Barriers to the blood pressure control appear to exist at patients, physicians and system levels. Poor knowledge of the disease and its management and poor adherence to antihypertensive drugs are well-known patient factors for suboptimal blood pressure control. Poor adherence to therapeutic guidelines and inadequate understanding of therapeutic goals are major physician-related barriers., Furthermore, health care system and low socio-economic status may present a barrier to blood pressure control, as high costs of screening and treatment may hinder the optimal control of hypertension among the low socio-economic group.
Little is known about the barriers to the hypertension management in rural Chinese communities. The primary objective of this study was to determine the patient-related barriers to blood pressure control in a rural community in East China.
Methods
Patients
This study was approved by the Institutional Review Board of our hospital, and written consent form was obtained from all participants. Between January 2010 and May 2012, 556 hypertensive patients were interviewed for the management of hypertension. These patients were selected from those who attended the free health check clinics in our hospital after a radio and television advertisement. All patients had lived in Liaocheng City, a regional city in the south-west of Shandong Province of China, for more than five years. After obtaining medical history, a full physical examination including blood pressure measurements were conducted in all patients. An electrocardiogram and blood biochemistry tests were also performed. Information on patient's antihypertensive treatment, in particular the use of antihypertensive medications was collected.
Blood pressure was measured with the patient in a sitting position after 10 min of resting, using a mercury sphygmomanometer. Phase V Korotkoff sounds was used to determine the diastolic blood pressure. Hypertension was defined as either systolic BP e” 140 mm Hg or diastolic BP e” 90 mm Hg.
Interview questionnaires
The questionnaires during the interview were comprised of four categories. The first was in relation to formal education on hypertension provided by health professionals, either doctors or nursing staff during visits to hospitals or clinics since the first diagnosis of the disease. Patients were also asked whether they had sought information from social media in particular the Internet about hypertension and related cardiovascular risk factors.
The second part of the questionnaire was about the patient's knowledge on hypertension, on the optimal level of blood pressure and on the consequences of uncontrolled hypertension. Patients were asked to name two or more of the hypertension-related complications, such as coronary heart disease, stroke, renal failure, or eye disease (retinopathy).
Access to health care was assessed by asking whether patients had difficulties in making regular appointments to visit a cardiologist due to the unavailability of the doctor. They were also asked if financial concerns were a factor in preventing them to see a specialist on a regular basis.
Two questions were asked to evaluate medication adherence or compliance. The first was whether patients had forgotten to take antihypertensive drugs at least on three occasions each week in the 4-week period prior to the interview. They were also asked if they had omitted antihypertensive drugs because of the costs of the medications.
Statistical analysis
Data are expressed as means + standard deviation (SD) or percentages as appropriate. Comparison of numerical data between patients who were aware and unaware of the presence of hypertension was performed with an un-paired student t test, whereas analysis of categorical data between the two groups was performed with Chi-square of Fisher's exact test. P <0.05 was considered statistically significant. SPSS software was used for the statistical analysis.
Results
General findings
The general characteristics of the patients are shown in table 1. The median age of the patients was 63 years, with more males (n=365, 65.7%) than females (n=191, 34.3%). Current cigarette smokers were confined to male patients (126/365, 34.5%), with an overall smoking rate of 22.7% (126/556) of the entire patient population. Type 2 diabetes was present in 101 (18.2%) patients, and more than half of the patients (296, 53.2%) had dyslipidaemia. In addition, 82 (14.8%) patients had a history of coronary artery disease.
Table 1
| Indices | N (n=556) | % |
| Mean age (years) | 60.9 ± 10.1 (37–76) | - |
| Sex - male | 365 | 65.7 |
| Smoking | 126 | 22.7 |
| Alcohol consumption | 293 | 52.7 |
| Overweight/Obese (BMI > 25kg/m2) | 137 | 24.6 |
| Type 2 diabetes mellitus | 101 | 18.2 |
| Dyslipidaemia | 296 | 53.2 |
| Coronary artery disease* | 82 | 14.8 |
| Family history of hypertension | 269 | 48.3 |
| Awareness of hypertension diagnosis | 429 | 77.2 |
Among the 556 patients, 429 (77.2%) were aware that they had been previously diagnosed with hypertension, while 127 (22.8%) patients did not know they had hypertension, although their blood pressure was >140/90 mm Hg on two separate measurements in our clinics.
Management of hypertension
Patients who were unaware of the presence of hypertension at the time of this study did not receive any antihypertensive therapy. Their mean systolic and diastolic blood pressure was 167.3 ± 13.2 and 90.5 ± 7.8 mm Hg, respectively, which were higher than the mean systolic (159.3 ± 11.2 mm Hg, p = 0.001) and diastolic (81.2 ± 5.9 mm Hg, p = 0.017) blood pressure in the patients who were aware of the presence of hypertension (table 2).
Table 2
Comparison of the patients who were aware or unaware the presence of hypertension
| Indices | Aware (n=429) | Unaware (n=127) | P value |
| Mean age (years) | 60.2 ± 9.3 | 59.9 ± 10.2 | 0.466 |
| Sex - male | 287(66.9%) | 78(61.4%) | 0.287 |
| Mean SBP (mm Hg) | 159.3 ± 11.2 | 167.3 ± 13.2 | 0.001 |
| SBP> 140 mm Hg | 369(86.0%) | 125 (98.4%) | 0.001 |
| Mean DBP (mm Hg) | 87.9 ± 6.4 | 96.0 ± 7.1 | 0.017 |
| DBP > 90 mm Hg | 166(38.7%) | 72(56.7%) | 0.03 |
| BP <140/90 mm Hg | 54 (12.5%) | 0 (0%) | 0.001 |
| Antihypertensive medications | |||
| 0 medication | 206(48.0%) | 127(100%) | 0.001 |
| 1 medication | 161(37.5%) | 0 | 0.001 |
| 2 medications | 62(14.5%) | 0 | 0.001 |
In patients who were aware of the hypertension, 369 (86.0%) had a systolic blood pressure of 140 mm Hg or higher, and 166 (38.7%) had a diastolic blood pressure of 90 mm Hg or higher. The total number of the patients who had a blood pressure of less than 140/90 mm Hg in this group was 54 (12.5%) (table 2). The mean systolic and diastolic blood pressure the patients who were unaware of the presence of hypertension was 167.3 ± 13.2 and 96.0 ± 7.1 mmHg, respectively (table 2).
In patients who were aware of hypertension, 206 (48.0%) were not on any antihypertensive medication at the time of this study. In those who were treated with antihypertensive medications, most (161/223, 72.2%) were treated with one antihypertensive drug (table 2). None of the patients who were unaware of hypertension were treated with antihypertensive medications (table 2).
Patient related barriers to hypertension management
The potential barriers to optimal hypertension control in patients who were aware of the presence of hypertension are listed in table 3. Only 21 (4.9%) patients received formal counselling or education from health professionals since the first diagnosis of this disease. One hundred and twelve (26.1%) patients sought information on hypertension and related cardiovascular risk factors from social media, mostly the Internet. Only 74 (17.2%) of the patients were aware of the optimal level of blood pressure, and 86 (20.0%) could name two or more major risks or complications from hypertension, such as coronary heart disease, stroke or renal failure.
Table 3
Barriers to blood pressure control in patients who were aware of the presence of hypertension
| Indices | Number of patients (n=429) |
| Education on hypertension | |
| Counselling from health professionals | 21 (4.9%) |
| Self-education from social media | 112 (26.1%) |
| Knowledge on hypertension | |
| Knowing the optimal level of BP | 74 (17.2%) |
| Knowing two or more complications of hypertension | 86 (20.0%) |
| Access to health care | |
| Difficulties in visiting a cardiologist due to the unavailability of the doctor | 126 (29.4%) |
| Difficulties in visiting a cardiologist due to costs | 176 (41.0%) |
| Medication compliance | |
| Forgetting to take the regular antihypertensive drugs in the past 4 weeks | 279 (65.0%) |
| Omitting prescribed antihypertensive drugs due to the costs | 169 (39.4%) |
The access to a specialist doctor was assessed in two aspects. Difficulties in getting an appointment to see a cardiologist was reported by 126 (29.4%) patients, and financial concerns preventing them to see a specialist was found in 176 (41.0%) patients. In 279 (65%) patients, missing regular antihypertensive medications was reported in the 4-week period prior to this study. Omitting prescribed antihypertensive drugs due to the costs was reported by 169 (39.4%) patients.
Discussion
The main findings of this study were: a) Approximately 23% of the patients from this rural population were unaware of the presence of hypertension, and received no antihypertensive therapy; b) In patients who were aware of the presence of hypertension, 48.0% were not using any antihypertensive medications at the time of this study, and only 12.5% achieved optimal blood pressure control; c) Less than 5% of the patients who were aware of the presence of hypertension received formal counselling on the disease from the health professionals; d)Less than 20% of the patients had adequate knowledge of the complications or therapeutic targets of hypertension; e) Poor adherence to prescribed antihypertensive medications was common; f) Financial constraints appeared to be a factor hindering doctor visits and adherence to prescribed antihypertensive drugs.
Optimal blood pressure control in hypertension patients appears to be a long-standing challenge around the world. Earlier studies showed that less than 25% of patients who were treated for hypertension achieved the target blood pressure of less than 140/90 mm Hg., In China, less than 5% of treated hypertensive patients had blood pressure below 140/90mm Hg., The proportion of patients achieved optimal blood pressure in the present study was 12.5%, which was consistent with the abovementioned reports.
The suboptimal control of blood pressure is related to a number of factors. Failure to diagnose high blood pressure in clinics and hospitals is a major cause. Our earlier study on a rural Australian population showed that 56.7% of the patients with elevated blood pressure were unaware of the presence of hypertension. In the present study on a rural population in China, the unawareness was 22.8%. Patients who were unaware of the hypertension received no antihypertensive therapy, and had a higher level of systolic and diastolic blood pressure than those who knew they had hypertension.
Structured education on the management of hypertension and life style modification has been shown to facilitate body weight reduction and pharmacological control of blood pressure., Education and counselling on the nature of hypertension and its impact on health appeared inadequate in the present study, and this may have contributed to the overall poor control of hypertension. Only 4.9% of the patients received formal counselling from health professionals, and only 20% of the patients had adequate knowledge about the risks and complications from uncontrolled hypertension.
Patients' poor adherence to prescribed antihypertensive medications has been identified as one of the main reasons for uncontrolled hypertension., The poor medication adherence can be due to a number of factors, such as multiple dose regimens, poor eye sights or hands disabilities in the elderly,, or in some countries, financial constraints. In the present study, 65% of the patients reported poor medication adherence in the 4-week period prior to the interviews at our clinics. Although the specific causes of poor medication adherence in our patients were unclear, affordability of the medications played a part. In 39.4% of the patients, costs of the medications were a contributing factor for omitting the antihypertensive drugs. These results suggest that new strategies or policies need to be developed to reduce the costs of antihypertensive medications, and to ultimately improve the medication adherence.
It was important to note that 29.4% of our patients reported to have difficulties in accessing a specialist doctor due to unavailability of the doctors, and 41% reported costs were a hindering factor for the specialist visits. These results were somewhat surprising because in China in general, and in the city of Liaocheng where the study was conducted in particular, the health care system was based on a fee-for-service system, and the patients had the freedom of choosing specialist doctors at either municipal, district or community hospitals. Access to specialists has not been perceived as a major problem for hypertension treatment in the past. However the results of this study clearly indicate that there is a need to addressing the accessibility to specialist care, by either enhancing the availability of the specialist services, or containing the costs of these services, or both.
Conclusion
The present study has found that in the majority of the patients with hypertension from this rural Chinese community, blood pressure was poorly controlled. The reasons for the suboptimal hypertension management are multifactorial. Potential barriers are inadequate education from health professionals, limited access to specialist care and poor adherence to antihypertensive medications. New strategies or policies are required to improve the patient's accessibility to specialist services, and to reduce the financial burden associated with the management of hypertension.
References
Reasons Why A Simpler Blood Pressure User Manual Is Imperative In Hindi
Clinical Scenario
A woman, age 72 years, has blood pressures of 150/70 mm Hg and 150/80 mm Hg, obtained by a medical assistant (MA), on consecutive office visits and does not have a history of hypertension. The blood pressure cuff is properly sized, the MA is inquiring about the patient's last mammogram while obtaining the blood pressure, and the patient is helping to hold her arm up within the MA's grasp. The mean of a dozen blood pressure readings that the patient has obtained at home is 128/64 mm Hg. Does this patient have white-coat hypertension?
Discussion
The most important commonly performed office test is blood pressure measurement, yet it is considerably undervalued. In the Kaiser Permanente Southern California (KPSC) Region, more than 2,300,000 blood pressure measurements were obtained by office staff in March 2009 (Ralph S Vogel, PhD, personal communication, 2009 April).a MAs often work in a rushed atmosphere, and physicians want their patients to be roomed promptly. However, populationwide, small inaccuracies in blood pressure measurement can have considerable consequences. Underestimating true blood pressure by 5 mm Hg would mislabel more than 20 million Americans with prehypertension when true hypertension is present. It has been predicted that the consequences of an untreated 5 mm Hg of excessive systolic blood pressure would be a 25% increase over current levels of fatal strokes and fatal myocardial infarctions for these individuals. Conversely, overestimating true blood pressure by 5 mm Hg would lead to inappropriate treatment with antihypertension medications in almost 30 million Americans, with attendant exposure to adverse drug effects, the psychological effects of misdiagnosis, and unnecessary cost.
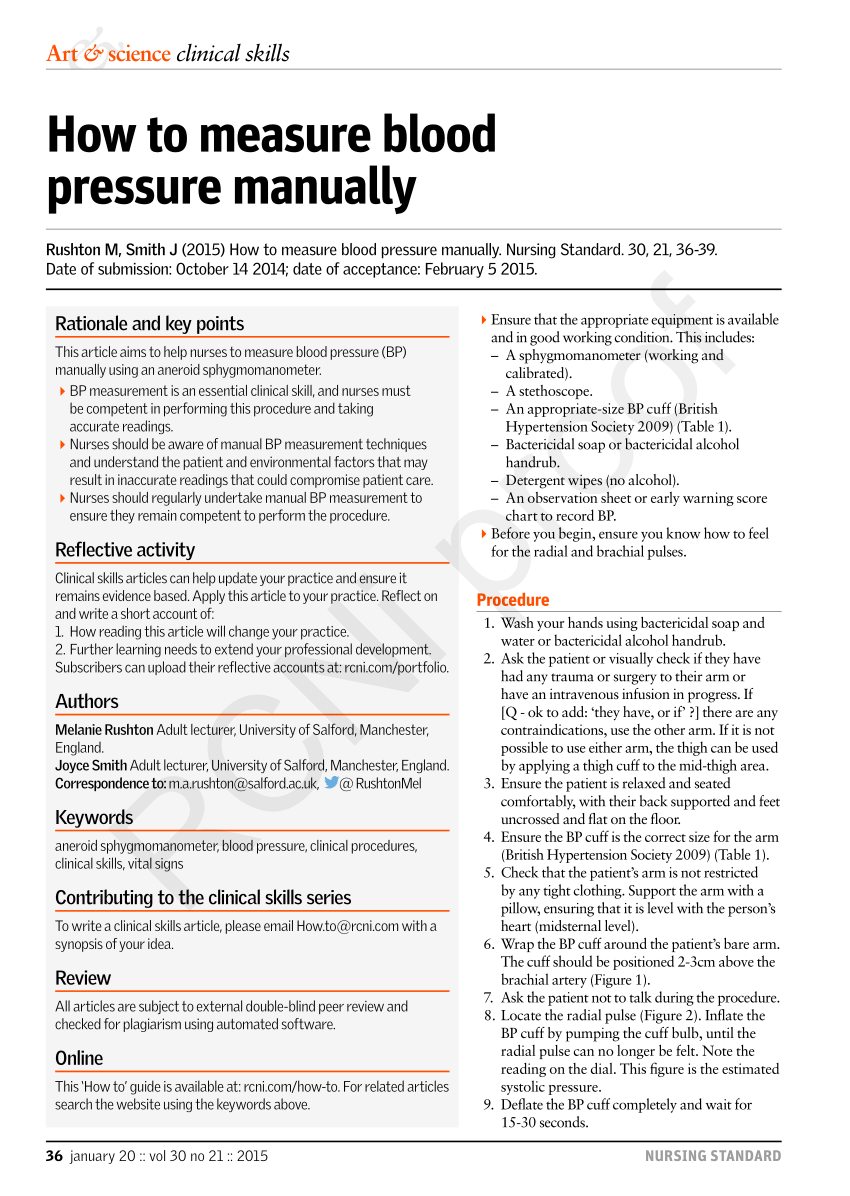
The trap is that in acknowledging the consequences of small measurement inaccuracies, errors of 5 to 10 mm Hg commonly occur as a result of improper blood pressure technique. Table 1 lists blood pressure aberrancies as a result of common errors. For example, active listening by the patient, when the MA is talking during blood pressure measurement, can increase systolic blood pressure by 10 mm Hg. Obtaining a measurement from an unsupported arm can increase the systolic pressure by 10 mm Hg. Lack of back support and crossed legs increase blood pressure. If a patient needs to urinate, a blood pressure measurement taken before bladder emptying can increase the systolic pressure by >10 mm Hg. Measurements taken over clothing or with tight clothing pushed up on the arm, causing a tourniquet effect, also produce significant artifacts. However, although many textbooks state that the bell of the stethoscope is more reliable than the diaphragm, studies show that is not the case., The commonplace use of the diaphragm side of the stethoscope is satisfactory. Figure 1 illustrates the proper technique for obtaining a sitting blood pressure.
Proper performance of a sitting blood pressure measurement. Note a proper-size cuff over a bare upper arm, which is positioned at heart level and supported on a table; the patient's back is supported and her feet are on the floor.
Table 1
Factors affecting accuracy of blood pressure measure
| Factor | Magnitude of systolic/diastolic blood pressure discrepancy (mm Hg) |
| Talking or active listening | 10/10 |
| Distended bladder | 15/10 |
| Cuff over clothing | 5–50/ |
| Cuff too small | 10/2–8 |
| Smoking within 30 minutes of measurement | 6–20/ |
| Paralyzed arm | 2–5/ |
| Back unsupported | 6–10/ |
| Arm unsupported, sitting | 1–7/5–11 |
| Arm unsupported, standing | 6–8/ |
… overestimating true blood pressure by 5 mm Hg would lead to inappropriate treatment with antihypertension medications in almost 30 million Americans, with attendant exposure to adverse drug effects, the psychological effects of misdiagnosis, and unnecessary cost.
Terminal Digit Preference
Terminal digit preference, a common source of error during manual blood pressure examinations, is the rounding off of numbers to the nearest zero. Usually the result is an inappropriate increase in the diagnosis of hypertension because systolic pressures in the upper 130s are rounded up to 140 mm Hg. In a KPSC blood pressure survey, 22% of recorded blood pressure numbers ended in zero; the expected occurrence would be 10%. Those results are better, however, than those from one literature survey, which reported that 78% of recorded blood pressure numbers terminated in zero., Although studies have been reported showing that an automated oscillometric device that provides five serial blood pressure measurements reduces the white-coat effect compared with manual determinations,, another study has shown that blood pressure is underestimated by this device, leading to significant misclassification of hypertension. The use of an automatic blood pressure monitor does have the advantage of obviating terminal digit preference, but the plethora of potential patient preparation errors still remain.
“… if the standing blood pressure is consistently much lower than the sitting blood pressure, the standing blood pressure should be used to titrate drug doses during treatment.”
Forearm Blood Pressure
What about taking a forearm blood pressure on an obese patient? Nurses often find that it is faster and easier to take a forearm blood pressure than to search for a larger cuff. Studies have shown that forearm blood pressures generally run 3.6/2.1 mm Hg higher than upper arm blood pressures., The experience in KPSC has been that once clinicians and MAs are taught how to obtain forearm blood pressures, inappropriate usage of forearm pressures becomes commonplace. Therefore, we no longer teach this technique. Instead, the regional mandate is to have both standard and large blood pressure cuffs in every primary care examination room. Using a standard blood pressure arm cuff on an obese patient falsely raises systolic blood pressure by approximately 10 mm Hg. “Miscuffing” should be strongly discouraged.
Proper Technique
For which patients is a standing blood pressure measurement most appropriate, and what is the proper technique for obtaining one? Particularly in patients who are ≥70 years old and taking antihypertension medications, obtaining standing blood pressure measurements should be routine practice. Although the sitting blood pressure measurement represents the standard in hypertension treatment trials, standing systolic pressure decreases of ≥20 mm Hg, consistent with a diagnosis of orthostatic hypotension, commonly occur and raise safety and quality-of-life issues in geriatric patients already at risk for dizziness and falling. Therefore, the National High Blood Pressure Working Group report on Hypertension in the Elderly concluded “… if the standing blood pressure is consistently much lower than the sitting blood pressure, the standing blood pressure should be used to titrate drug doses during treatment.” An international neurology consensus statement endorsed waiting “within three minutes” in the standing position and others have clarified this recommendation as being three minutes, but the protocol used in the landmark HYpertension in the Very Elderly Trial (HYVET) waited two minutes. Having patients stand for two to three minutes before their upright blood pressure measurement is taken is reasonable for hypertension management. When blood pressure is properly measured in the standing position, the arm should be supported (Figure 2). When measurement is taken on a dangling arm, the systolic pressure may artifactually be 6 to 10 mm Hg higher than in an arm that is properly supported.,
Proper measurement of a standing blood pressure requires complete arm support with cuff at heart level. Hold the arm if an adjustable table is unavailable.
Doctor or Nurse or Medical Assistant
Who should be measuring the blood pressure after all, physician or nurse? In all of the hypertension treatment trials, blood pressure has been measured by trained nonphysicians, usually nurses. White-coat effect is common and persistent. In a classic study of nurse and physician blood pressures undertaken in patients with continuous intra-arterial blood pressure monitoring, two concurrent measurement phenomena were observed: observer effect and alerting reaction (Figure 3). After a few minutes, a repeat blood pressure measurement obtained by both a physician and a nurse produced results about 10/5 mm Hg lower than the first determination, owing to mitigation of the alerting reaction. Nonetheless, there was a difference of 10/5 mm Hg between the physician and the nurse with both the first and second determinations, demonstrating the persistence of the observer, or white-coat, effect. Patients are more afraid of physicians than of nurses. If an initial blood pressure reading obtained by an MA is elevated and a physician then obtains a follow-up reading, that second reading may be lower because the alerting reaction has subsided, or it may be higher because of doctor-related white-coat effect. Physicians taking blood pressure measurements should be knowledgeable regarding proper technique and the causes of artifacts.
Demonstration of relative blood pressure alerting reactions and observer effects, comparing physician and nurse.
ΔSBP = change in systolic blood pressure, ΔDBP = change in diastolic blood pressure. Reprinted with permission from Mancia G, Parati G, Pomidossi G, Grassi G, Casadei R, Zanchetti A. Alerting reaction and rise in blood pressure during measurement by physician and nurse. Hypertension 1987 Feb;9(2):209–15.
Multiple competent blood pressure measurements by MAs can obviate the white-coat effect. Two studies have shown that several measurements obtained by nurses can approximate mean blood pressure measurements obtained by 24-hour ambulatory blood pressure recordings., The discrepancy between office blood pressure measurements and 24-hour ambulatory measurements is at least in part because of poor office competence in obtaining accurate readings. When there is concern regarding the possibility of the white-coat effect, having MAs obtain weekly blood pressure measurements for two weeks should be considered. Whenever the first blood pressure reading is elevated, a second reading should be obtained after a one-minute interval.
Patients
Patients are increasingly helpful as quality-assurance monitors. Educational materials are available to teach proper home blood pressure measurement technique, and other general patient-education materials demonstrating blood pressure measurement competency have been distributed. On a few occasions, we have received accurate criticism of blood pressure measurement technique performed by our staff from patients in KPSC. Also, peer-validator competency review of blood pressure measurement by
MAs is expanding in our system: MAs receiving peer-validator training offer critiques and instruction to their colleagues in a program that has generated positive feedback from participants. Additionally, a new blood pressure measurement training video is being developed, with “train-the-trainer”8 Webinars planned for later in 2009.
Conclusions
The patient whose case was presented at the beginning of this article does not have hypertension despite the elevated office readings, and she does not need home blood pressure measurements for a diagnosis of white-coat hypertension to be made. White-coat hypertension indicates a dissociation between competently determined office blood pressure elevations and normal blood pressure readings obtained at home. Therefore, findings for this patient do not qualify for a diagnosis of white-coat hypertension, because the office blood pressure readings are inaccurate. Terminal digit preference is a marker of inaccurate office technique: all four office measurements for the patient ended in zero. Active listening by the patient, from whom medical information was requested during blood pressure measurement, and partial patient support of her outstretched arm could easily have accounted for a systolic artifact of >10 mm Hg. This patient was exposed to the possibility of receiving an inaccurate diagnosis of hypertension and taking inappropriate antihypertension medications. Her case illustrates potential patient care problems ensuing from poor office blood pressure measuring technique.
If an initial blood pressure reading obtained by an MA is elevated and a physician then obtains a follow-up reading, that second reading may be lower because the alerting reaction has subsided, or it may be higher because of doctor-related white-coat effect.
Take a minute to examine Figure 4 and list all ten errors in obtaining the sitting blood pressure shown. (Key to answers listed below.)
What is wrong with the blood pressure measurement technique in this picture? Can you list all ten errors? (Key to answers on page 54.)
Figure 4. What is wrong with the blood pressure measurement technique in this picture? Key for errors:1) Patient's arm is unsupported; 2) Patient's back is unsupported; 3) Patient is talking; 4) Patient is engaged in active listening; 5) Wrong size cuff in use (“miscuffing”); 6) Blood pressure cuff is positioned too low on the upper arm; appears to be over the elbow; the artery marker on the cuff is probably malpositioned as well; 7) Cuff is over clothing; 8) Observer is not at eye level with the monitor; where is the monitor? 9) Patient's legs are crossed; 10) End of stethoscope is in clinician's coat pocket.
Footnotes
a Practice Leader, Data Consulting and Report Production, Southern California Permanente Medical Group Clinical Analysis
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
Acknowledgments
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
References

Reasons Why A Simpler Blood Pressure User Manual Is Imperative Theory
Reasons Why A Simpler Blood Pressure User Manual Is Imperative In Spanish